What are the most common types and sites of injuries in surgeons? Is my specialty at risk?
It Can Happen to You
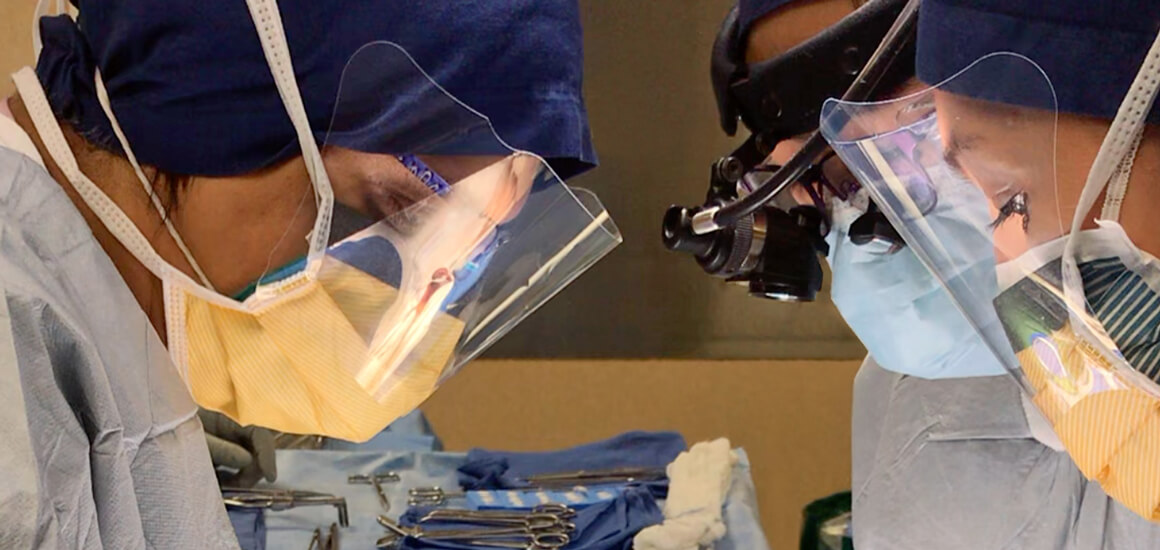
“Can you sniff the incision? Does it smell good?” asked the Senior attending I was working with that day in my PGY2 year. I was perplexed at the query, so he proceeded to explain. “Your neck is bent so forward that you’re going to have a lot of pain at the end of the day. Stand up straight when you’re operating”. My fellow residents and I heard this refrain every once in a while. We also saw several older attendings with permanent stoops and heard of others who had to retire early due to pain or other injuries sustained during the course of their careers. We’d whisper to each other “Must’ve been something else, not operating”, in addition to thinking that it wouldn’t happen to us. Call it naivete, the resilient bodies of our youth or whatever else you’d like, but it is crucial to know that surgeons can absolutely develop WRMSD.
In fact, large meta-analyses show that surgeons report several work-related symptoms including pain, fatigue, stiffness and numbness. The most common locations for pain are the neck, back, arms/shoulders and hands. Moreover, no surgical specialty is immune. WRMSDs have been reported in almost all areas of surgery, and surgeons performing endoscopic or minimally invasive procedures have the greatest risks (when compared to open procedures). In addition, female surgeons have much higher rates of symptoms even after controlling for glove size, height and years in practice. Not surprisingly, the most common types of injuries reported include degenerative disease of the cervical or lumbar spine, rotator cuff pathology and carpal tunnel syndrome.
So, the next time you’re operating as a trainee or a full-fledged surgeon, remember to think about how you can improve the ergonomics of your task because…it can very well happen to you.
Interested in learning about other injuries that can result from poor ergonomics? Invite Dr. Lal to speak at your next conference.